Medical Intensive care unit (MICU) patients are exposed to radiation higher than annual US Federal occupational standard limits within a short period of time during radioscopic studies. Research conducted between January and December 2013 by scientists at the Cleveland Clinical Foundation discovered this to be true among 3% of the total 4155 patients involved in the study.
The millisievert (mSv) is a measure of the organic effect of ionizing radiation and is known as the effective dose (ED). Statistical tests conducted on the data obtained in the study showed that 36% of the patients were exposed to radiation higher than the natural background radiation (~3 mSv). Values just 3-5 times higher have been suspected to cause carcinogenesis, although the debate is still ongoing.
Radiation is used in numerous reliable diagnostic procedures in the MICU. Although this has been overshadowing the potential risk of cancers, recently, more medical literatures are exploring its adverse effects. The study also showed an increase in cumulative ED for patients with a higher length of stay at the MICU. Among the radiation based Imaging systems used in healthcare, CT and IR caused the highest amount of radiation burden. However, diagnosis of sepsis, COPD, cirrhosis and Gastrointestinal bleeding were seen to affect cumulative ED.

Ionizing radiation can lead to cancers by damaging our DNA or RNA, and cause genetic abnormalities. This is especially true for kids and young adults who have a high rate of cellular division and a longer lifespan to express the effects of radiation. Krishnan et al report that despite their adoption of the ALARA (‘as low as reasonably achievable’) principle of radiation safety, patients were exposed to substantial amounts of radiation during diagnosis. Therefore, they suggest methods for assessing the risk vs benefit of radiation therapy.
“Proactive monitoring of CED with real time display in electronic medical resorts will assist physicians in deciding the risk-benefit ratio.”
The study was limited as it was conducted among MICU patients from a single academic medical center. The estimate of ED from previous papers and the limited medical records from which data was obtained could have caused an undervaluation of the cumulative ED. Another shortcoming was the disregard for patient basic characteristics like age and sex. Nevertheless, the results denote a need to conduct more research to weigh the pros and cons of radiation in medicine and its effects on overall patient health.
This makes me wonder, are we so highly dependent on radioscopic resources that we fail to consider the harm it might be doing us? At this day and age of technological advancement, there should be active endeavors to explore the benefits and possible disadvantages of radiation in the medical industry and ways to alleviate them.
Reference: Krishnan S, Moghekar A, Duggal A, Yella J, Narechania S, Ramachandran V, Mehta A, Adhi F, Vijayan AKC, Han X, Dong F, Martin C III, Guzman J, Radiation Exposure in the Medical Intensive Care Unit- Predictors and Characteristics, CHEST (2018), doi: 10. 1016/ j.chest.2018/01/019.
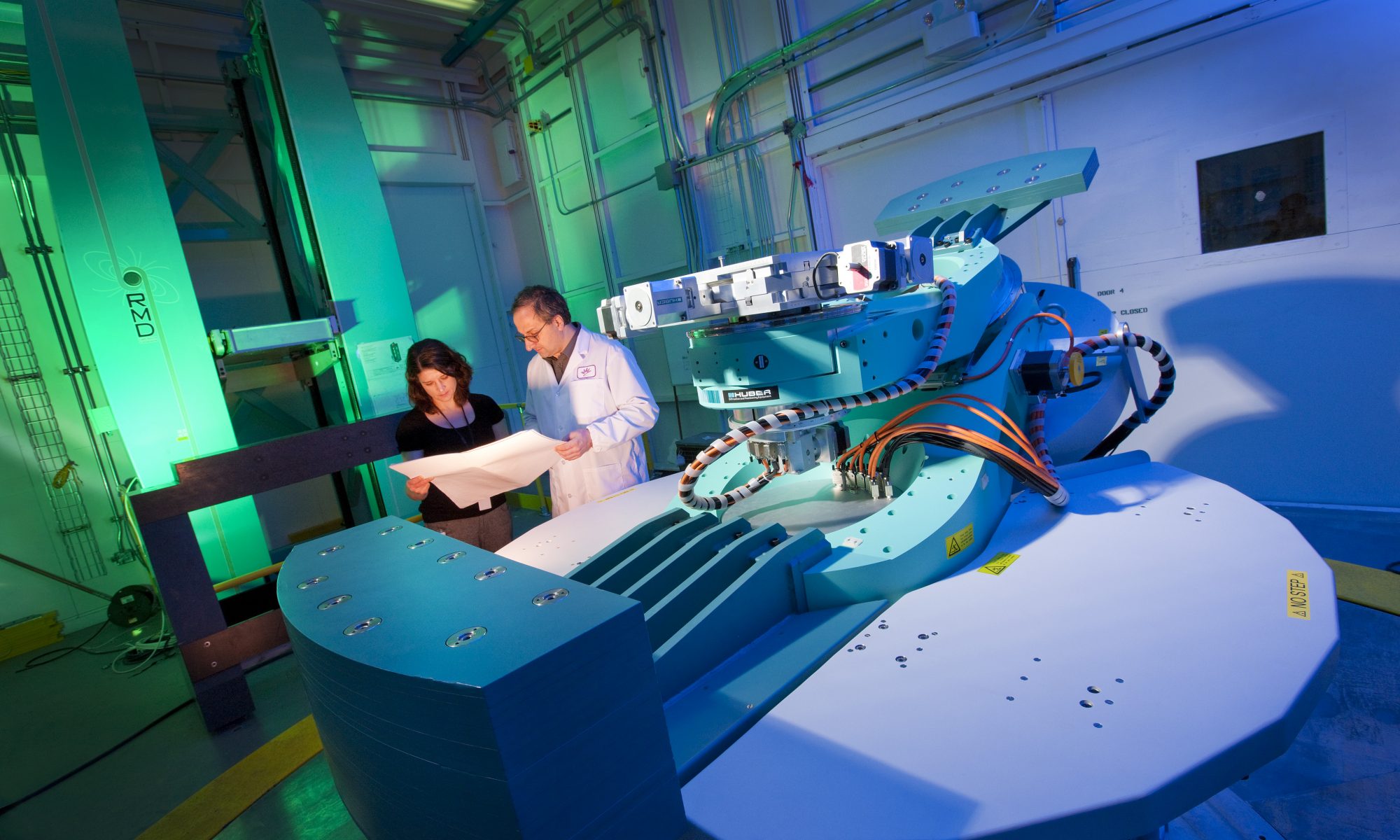
Canadian Light Source Research Office

I appreciated the clinical relevancy of this article, and especially the question you posed at the end about whether or not a clinical dependence on radiation for diagnostic testing is skewing the medical professionals’ perception of benefit vs harm to a patient. I also liked the graph in the middle because it gave a more practical sense of where the radiation is coming from in a treatment or diagnostic scenario.
Interesting article! I had a similar question to the hyper-use of radiative technology, especially with phones. Are there other test that can be used that do not use radiation?