Antibiotic resistant bacteria are frightening. When resistant, the bacteria are not affected by the drugs usually employed to kill them (antibiotics). Some postulate that such “superbugs” might even spell the end for humanity in the too-near future. To study bacterial resistance, Nathalie Q. Balaban from the Hebrew University of Jerusalem and fellow infectious disease experts tracked the evolution of methicillin-resistant Staphylococcus aureus (MRSA, pronounced mur-suh) extracted from the blood of infected patients at the Shaare Zedek Medical Center. In their January 2020 Science article, they explore MRSA resistance under combinations of the antibiotic treatments rifampicin (RIF) and daptomycin (DAP).

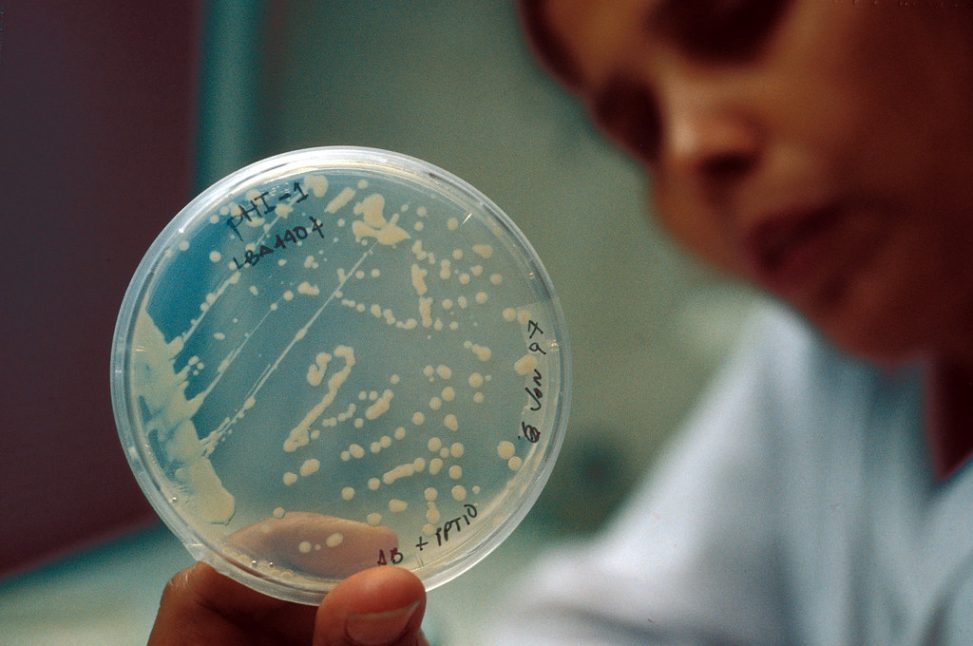
“The Illusion of Drugs” by Eyad Elbayoumi is licensed under CC BY 2.0
In one patient, MRSA developed resistance to RIF after receiving the combination of DAP and RIF antibiotics. This was not good news since combination treatment should, in theory, help prevent resistance. However, the finding helped the researchers discover more information about the evolution of bacteria.
Before resistance develops, bacteria could acquire tolerance mutations. When tolerant, bacteria become temporarily dormant (i.e. stop growing) to evade the effects of antibiotic treatment, which only functions on actively growing bacteria. Tolerance lasts a few days and is called the tolerance window. Since RIF reduces DAP’s killing power and is therefore considered suppressive, an initial DAP treatment was shown to work more effectively than the combination of RIF and DAP. The results suggest that doctors should first prescribe DAP only, ideally before the tolerance window.
“We observed that bacteria acquired tolerance within a few days. These tolerance mutations then acted as a stepping stone to acquire resistance and, ultimately, treatment failure,” described Balaban.
Balaban highlighted the importance of treating patients not just before resistance develops, but also before tolerance develops. The results indicate a counterintuitive approach: monotherapy might could be more effective than combination therapy. Balaban’s conclusions suggest that antibiotics don’t necessarily need to become stronger, but instead just prescribed more effectively. Further, the findings could improve both the prescription patterns of doctors and patient prognoses.
“Using the right combination of available antibiotic drugs at the outset could dramatically increase a patients’ survival rate before their infection becomes tolerant to all the antibiotics in our arsenal,” Balaban concluded.
Thanks to the work of Balaban and colleagues, the superbug apocalypse might just have gotten a rain check.
Citation
Liu J, Gefen O, Ronin I, Bar-Meir M, Balaban NQ. 2020. Effect of tolerance on the evolution of antibiotic resistance under drug combinations. Science 367: 200–204.
Alex
"This title was very eye catching! That is so interesting that such a ..."
Alex
"This is really interesting! The fact that crops and plants are damaged is ..."
Alex
"Well done, this article is great and the information is very captivating! Ethics ..."
Alex
"I was intrigued throughout the whole article! This is such an interesting topic, ..."
Alex
"This is such an interesting article, and very relevant!! Great job at explaining ..."
Grandpa
"Honey You Did a good job I will forward to my eye doctor "
murphymv
"This article is fascinating because it delves into the details of the research ..."
murphymv
"I agree, adding the photo helped solidify the main finding. "
murphymv
"This is a fascinating finding. I hope this innovative approach to improving transplants ..."
Sherzilla
"This is a great article! I would really love to hear how exactly ..."
Sherzilla
"It's disappointment that these treatments were not very effective but hopefully other researchers ..."
Sherzilla
"I agree with your idea that we need to shift our focus to ..."
Sherzilla
"It's amazing to see how such an everyday household product such as ..."
Lauren Kageler
"I will be interested to see what the data looks like from the ..."
Lauren Kageler
"A very interesting article that emphasizes one of the many benefits that the ..."
maricha
"Great post! I had known about the plight of Little Browns, but I ..."
Sherzilla
"I assumed cancer patients were more at risk to the virus but I ..."
Sherzilla
"Great article! It sheds light on a topic that everyone is curious about. ..."
maricha
"This article is full of really important and relevant information! I really liked ..."
maricha
"Definitely a very newsworthy article! Nice job explaining the structure of the virus ..."
maricha
"It's interesting to think that humans aren't only species dealing with the global ..."
murphymv
"This is very interesting and well explained. I am not too familiar with ..."
Lauren Kageler
"Great article! This post is sure to be a useful resource for any ..."
Lauren Kageler
"Definitely seems like an odd pairing at first, but any step forward in ..."
murphymv
"What an interesting article! As you say, height and dementia seem unrelated at ..."
murphymv
"Great article! I learned several new methods of wildlife tracking. This seems like ..."
murphymv
"Very interesting topic! You explained cascade testing and its importance very well. I ..."
Alex
"This article is really interesting! What got me hooked right away was the ..."
Sabrina
"I found this article super interesting! It’s crazy how everyday products can cause ..."
Erin Heeschen
"I love the layout of this article; it's very eyecatching! The advancements of prosthetics ..."
murphymv
"Awesome article! I like the personality in the writing. Flash Graphene not only ..."
murphymv
"Very interesting work! I don't know a whole lot about genetics, but this ..."
Cami Meckley
"I think the idea of using virtual reality technology to better help prepare ..."
Erin Heeschen
"I wonder if there's a connection between tourist season and wildfires in the ..."
Ralph berezan
"Not bad Good work "
Michelle
"This sounds like it would be a great tool for medical students! ..."