In 2019, approximately 322,000 men died from cancer in the United States alone. The combination of lung cancer, prostate cancer and colorectal cancer made up about half of those deaths. As frightening as that number is, a significant percentage of each of these cancers can be successfully treated if caught early. Researchers are continuously working hard to develop better therapeutic options and new treatments for diagnosed patients. One group of scientists at Purdue University have created a new therapy option that may help halt tumor growth in certain cancers such as prostate, which is among the most common types of cancer in men.
The Purdue team used a protein called interleukin-27, or IL-27, which has previously shown promise in reducing tumor growth and helping stop cancer from spreading through the body. IL-27 is a cytokine, which is a type of protein secreted by cells of the immune system that act as chemical messengers. Normally, our immune system’s front line of defense (specific cells) scour our body looking for foreign bodies, e.g. viruses, bacteria or mutated cancer cells, and then when they identify something foreign, cytokines, such as IL-27, will be secreted. These cytokines signal for the immune system ‘fighters’ to recruit to the respective area to fight the foreign ‘enemy’ to our bodies. Recently, it was shown that IL-27 is involved in regulating an immune response against tumor development and in serving as an ‘alarm’ to sense inflammatory or infectious response to promote bone repair.
“Immune cells are naturally attracted to areas of the body with lots of signals that come from proteins such as IL-27,” Figueiredo, the lead researcher explained. “So, with our novel approach of targeting the IL-27 to the tumor or bone cells, we can use these proteins to produce signals that bring healthy cells to areas of the body with cancer or other disease and kill the tumors and begin the process of repairing bone and other musculoskeletal tissues.”
Knowing that IL-27 has the potential to recruit healthy immune cells to the tumor environment and consequently attack the tumor, the research team led by Dr. Figueiredo designed a method for the targeted delivery of this protein to the site of a tumor. The group developed a clinically safe sonoporation delivery method. Sonodelivery is the use of sound waves to modify the permeability of the cell membrane so that the drug, in this case targeted IL-27, can cross into the cell easier. Essentially, the sound waves disrupt the membrane surrounding specific cells, thus allowing the target to enter those cells and take action. Previous studies using this sonodelivery method to deliver wild-type IL-27, which is IL-27 as it normally occurs in the body, worked well to slow bone destruction and inhibited tumor growth in cancer patients. However, the tumor growth rate was reduced but not completely eradicated. Therefore, the researchers investigated an alternative route for getting IL-27 to tumor cells specifically: they hypothesized that they could direct the IL-27 to tumor tissue by using peptides (small proteins) that could bind to receptors that are upregulated in tumor cells, thus augmenting IL-27 bioactivity. Essentially, Figueiredo and his group attached a new protein to IL-27 molecules, knowing that this specific protein (which you can think of as a key) binds well to a receptor (which you can think of as the lock) that is present in high abundance in tumor cells.
This method is also beneficial because it allows for the treatment to be specific to cancer cells: their preliminary results suggested that this peptide, named pepL, is effective in the body to target and treat aggressive prostate tumors, since the receptor for it is upregulated (present in higher numbers) in ~95% of prostate cancer tumor metastases relative to normal tissues. Moreover, the peptide+IL-27 combination showed a ~10- to 13-fold increase in binding to tumor cells compared to normal control cells.
Most importantly, the engineering that they conducted to join IL-27 with pepL resulted in higher bioactivity of the cytokine in the body relative to a non-specific control peptide. The tumor growth inhibition was significant in tumors treated with just IL27 (~50%) but further enhanced to an 89% growth inhibition in IL-27+pepL treated tumors. This is a remarkable difference!
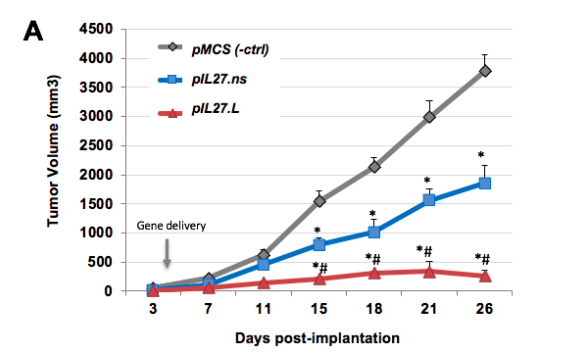
Graph showing that the targeted IL-27 with the peptide (red) caused a significant decrease in tumor growth compared to IL-27 alone (blue) and no IL-27 (grey).
Not only did this new method target the IL-27 chemical signaler to the tumors more specifically, but the activity of IL-27 was also enhanced, allowing for a stronger immune response against tumor cells. Additionally, the researchers found that IL-27 can impact both the targeted cell (tumor) as well as neighboring cells (bone cells or other tumor cells, for example).
There remains a lack of therapeutics that can simultaneously and effectively treat the prostate tumor while restoring affected bone tissue. Cytokine immunotherapies hold great promise because they are secreted molecules that can reach and treat both primary and distant secondary tumors. Thus, IL-27 targeting with pepL may augment cytokine bioactivity and success against prostate tumors in the body.
“This new therapy technology has applications for people and animals with many different types of cancer, including breast and lung, and other diseases where protein targeting could improve the immune system’s response,” according to Figueiredo.
M.L. Figueiredo, M. Figueiredo Neto, J.W. Salameh, R.E. Decker, R. Letteri, D. Chan-Seng, T. Emrick. Ligand-mediated targeting of cytokine Interleukin-27 enhances its bioactivity in vivo. Molecular Therapy – Methods & Clinical Development, 2020; DOI: 10.1016/j.omtm.2020.03.022
Alex
"This title was very eye catching! That is so interesting that such a ..."
Alex
"This is really interesting! The fact that crops and plants are damaged is ..."
Alex
"Well done, this article is great and the information is very captivating! Ethics ..."
Alex
"I was intrigued throughout the whole article! This is such an interesting topic, ..."
Alex
"This is such an interesting article, and very relevant!! Great job at explaining ..."
Grandpa
"Honey You Did a good job I will forward to my eye doctor "
murphymv
"This article is fascinating because it delves into the details of the research ..."
murphymv
"I agree, adding the photo helped solidify the main finding. "
murphymv
"This is a fascinating finding. I hope this innovative approach to improving transplants ..."
Sherzilla
"This is a great article! I would really love to hear how exactly ..."
Sherzilla
"It's disappointment that these treatments were not very effective but hopefully other researchers ..."
Sherzilla
"I agree with your idea that we need to shift our focus to ..."
Sherzilla
"It's amazing to see how such an everyday household product such as ..."
Lauren Kageler
"I will be interested to see what the data looks like from the ..."
Lauren Kageler
"A very interesting article that emphasizes one of the many benefits that the ..."
maricha
"Great post! I had known about the plight of Little Browns, but I ..."
Sherzilla
"I assumed cancer patients were more at risk to the virus but I ..."
Sherzilla
"Great article! It sheds light on a topic that everyone is curious about. ..."
maricha
"This article is full of really important and relevant information! I really liked ..."
maricha
"Definitely a very newsworthy article! Nice job explaining the structure of the virus ..."
maricha
"It's interesting to think that humans aren't only species dealing with the global ..."
murphymv
"This is very interesting and well explained. I am not too familiar with ..."
Lauren Kageler
"Great article! This post is sure to be a useful resource for any ..."
Lauren Kageler
"Definitely seems like an odd pairing at first, but any step forward in ..."
murphymv
"What an interesting article! As you say, height and dementia seem unrelated at ..."
murphymv
"Great article! I learned several new methods of wildlife tracking. This seems like ..."
murphymv
"Very interesting topic! You explained cascade testing and its importance very well. I ..."
Alex
"This article is really interesting! What got me hooked right away was the ..."
Sabrina
"I found this article super interesting! It’s crazy how everyday products can cause ..."
Erin Heeschen
"I love the layout of this article; it's very eyecatching! The advancements of prosthetics ..."
murphymv
"Awesome article! I like the personality in the writing. Flash Graphene not only ..."
murphymv
"Very interesting work! I don't know a whole lot about genetics, but this ..."
Cami Meckley
"I think the idea of using virtual reality technology to better help prepare ..."
Erin Heeschen
"I wonder if there's a connection between tourist season and wildfires in the ..."
Ralph berezan
"Not bad Good work "
Michelle
"This sounds like it would be a great tool for medical students! ..."