This image illustrates the connection between the brain and the gut’s nervous system, known as the “second brain.” eps 10
This week we examined the complex communication system between the gut and brain, otherwise known as the Gut-Brain Axis. The gut-brain axis is a bidirectional network that allows the central nervous system and the gastrointestinal tract to exchange signals through neural, hormonal, and immune pathways. The gut is a diverse microbiome that contains 168 neurons which connect to your brain through the nervous system. The microbes in the gut play a huge role in producing short-chain fatty acids which strengthen the intestinal barrier, reduce inflammation, and support the blood-brain barrier, ultimately affecting mood, cognition, and overall brain function.
What is the Gut Microbiome?
The gut microbiome consists of 100 trillion living bacteria within the body’s digestive tract that help digest food, produce essential vitamins, and regulate our immune system. In Genevieve Wanucha’s reading, the focus is on how the microbiome influences the brain. The bacteria in the gut produce neuroactive compounds such as serotonin, which helps to regulate our emotions and mood. Therefore, an unhealthy gut can have serious consequences on someone’s mental health. As Wanucha illustrates, “a diverse microbiome is a healthy one”, meaning that a rich community of various bacterial species is necessary to maintain balance and prevent one strain from dominating. Disruptions in this balance have been linked to diseases like autism, inflammatory bowel disease, blood cancers, and Alzheimers. The article also highlights that a person’s genetic makeup plays a major role in the health of their microbiome. While we can’t change our genes, we can improve our diet to help support a healthy gut. Implementing more fibrous, fermented, and probiotics and prebiotics foods can significantly strengthen the gut microbiota. By supporting a health gut environment, these dietary changes can enhance brain health and overall well-being.
Microbiome Development & Diversity
The gut microbiome is largely impacted by genetics and is significantly impacted by one’s parents. While in utero, a mother’s plays a crucial role in shaping her child’s microbiome. For example, eating nutrient-rich, fiber-heavy foods can promote beneficial bacteria, while a diet high in processed foods and sugar may lead to less diverse gut microbes. As the baby is developing in utero, their gastrointestinal track is developing as well, which is why doctors promote prenatal vitamins and health diets for mothers. The method of birth, vaginal or c-section, is another factor of how a child’s microbiome is affected by their mother’s. The mode of delivery influences the initial colonization of microorganism in infants. C-section babies often have a delay in the development of immune systems, whereas vaginal babies don’t experience that delay. To address this, some Hospitals will expose c-section babies to the organisms they did not receive from a vaginal birth. This helps to diversify the babies microbiome early on in development. Finally, feeding practices ,like formula or breast milk, shape an infant’s microbiome. Breast milk contains high levels of colostrum which is an antibody that helps build the infants immune system. Therefore, infants that were formula feed lack that colostrum and may experience differences in immune protection. An example talked about in class, was when Professor Halpin did her work in the Peace Corps, in Niger. Many natives discouraged breastfeeding, because they believe that breast milk was bad. They viewed mothers who did not breast feed as “wealthier”, because of this mother’s used cow milk. However, this practice contributed to one of the highest infant morbidity rates in the region due to the lack of antibodies found in breast milk.
Alzheimer’s and the Gut-Brain Connection
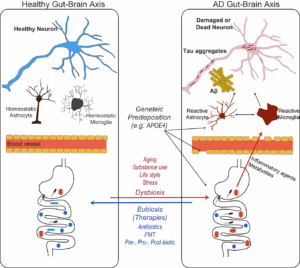
As mentioned above, disruptions to your microbiome are linked to diseases, one of the most common ones being Alzheimer’s disease. Research shows that individuals with Alzheimer’s have a less diverse and imbalanced community of gut microorganisms. According to the studies cited by Wanucha, “the microbiomes of people with Alzheimer’s diseases have specific increases and decreases in common gut bacteria, especially decreases in Bifidobacteirum, an important inhabitant of the health human gut” (Wanucha). Researchers are exploring ways to restore healthy gut bacteria in Alzheimer’s patients as a potential method to prevent or slow the disease. Targeted microbiome therapies have become popular in treatment, however since genetics play a huge role in shaping the microbiome, it is essential to consider a patient’s genetic background before treating.
References
Robertson, K. (2023, May 16). The gut-brain connection: How it works and the role of nutrition. Healthline. https://www.healthline.com/nutrition/gut-brain-connection
Seo, Do., Holtzman, D.M. Current understanding of the Alzheimer’s disease-associated microbiome and therapeutic strategies. Exp Mol Med 56, 86–94 (2024). https://doi.org/10.1038/s12276-023-01146-2
Tompa, Rachel. “Scientists Explore Role of Gut-Brain Axis in Parkinson’s, Anxiety, and Long COVID.” Stanford Report, 6 Mar. 2025, https://news.stanford.edu/stories/2025/03/gut-brain-research-long-covid-parkinsons-anxiety.
Wanucha, G. (n.d.). The gut microbiome and brain health. Memory and Brain Wellness Center, University of Washington. http://depts.washington.edu/mbwc/news/article/the-gut-microbiome-and-brain-health
Erin,
Your blog post provides lots of interesting insights into the significance of the gut-brain axis, connecting its role to various aspects of health. The link between the gut microbiome and immune health, genetics, hormones, and other biological functions is fascinating. One particularly interesting example we discussed in class was the difference in microbiomes between individuals with and without depression. Since about 95% of the body’s serotonin is produced in the gut, this may help understand why emotions are so closely connected to gut health. Furthermore, your post and our class describes the relationship between gut health, the microbiome, and external factors such as diet and the environment. The composition of the gut microbiome is influenced by what we eat and our surroundings, further underlining the importance of a balanced diet and a healthy lifestyle in maintaining optimal gut function. This connection between gut health and mental well-being offers an interesting new area of research for food studies scholars. The gut-brain axis truly demonstrates the profound impact of gut health on both physical and mental health.
Dear Erin,
Your blog post provides a strong summary of our class on the Gut-Brain connection and what we learned about the microbiome. Your inclusion of the reading from Wanucha to illustrate the connection between the microbiome and certain diseases such as Alzheimer’s helped me apply the overall information about the brain-gut axis to a specific health scenario. This area of research in particular is very interesting and I look forward to seeing how it continues to develop as a part of Food Studies. Pertaining to microbiome development, your section on how infants’ microbiomes differ depending on modes of birth and feeding expanded on a part of our class discussion that really interested me. Do you think that expanding education for new mothers about how their babies’ microbiomes and immune health will be impacted by these factors might lead to increased microbiome health overall? Personally, most of this knowledge is brand new, so it could be beneficial to emphasize understanding of microbiome health in early childhood for the general population.
Parker
Erin,
This is a great summary of the gut microbiome, its development, and its impact on the brain. You made this complex topic easy to understand and in a way that feels accessible to people outside of our class. You did a good job highlighting the importance of bacterial diversity and genetics in understanding the gut too. It was an important reminder that although we can’t change our genes, we can control our diet. I also liked your discussion of the development of the microbiome and the things mothers should be aware of during pregnancy (diet, prenatals, birth method, feeding method, etc.). Related to this, I think Parker brings up a great point about educating mothers. There is a lot of conversation about habits during pregnancy, particularly drug and alcohol use, but there is less talk on the impact mothers have on their babies’ guts. After having seen your digital story, I would be curious to know if and how this topic ties into athlete nutrition. We learned from the Nature article (“The microbiota–gut–brain axis”), that a balanced microbiome in mice increases anxiety-like behaviors and decreased depression-like behaviors. Given that these mental health factors likely play a role in athletes’ success, could a healthier microbiome boost performance?
Hi Erin,
Thank you for your post! The gut microbiome plays such a fundamental role in our lives, and hence is a very important topic to educate ourselves on. This awareness is particularly important given the variety of factors that influence its health and diversity. I found it interesting how such as seemingly unrelated factor as method of birth can directly impact gut health; this vividly illustrates the intense interconnectedness of the human body. Additionally, I believe more research is necessary to fully understand the ways in which the gut influences disease. As we discussed in class, disruptions in certain strains of bacteria are associated with different effects on the body. This was made clear in the Robertson article by Healthline. The article also discusses the importance of the vagus nerve to the gut-brain axis, providing a physical pathway between the gut and brain through the nervous system. A connection is also apparent in the gut’s production of neurochemicals. Given that over 90% of serotonin is produced in the gut, and as the most commonly used drugs to fight anxiety and depression are SSRIs which artificially increase the presence of serotonin in the brain, it is clear that serotonin production directly affects mental disorders. The gut has proven itself to be central to overall human health.
Claire