By Nick Gubitosi
 Just last week (April 6, 2010), scientists at the Rush University Medical Center in Chicago completed the second phase of trials for a very promising melanoma vaccine. The trial, which had stunning results, was conducted on 50 patients with metastatic melanoma, which is melanoma that had spread to multiple parts of the body. Currently treatments for advanced melanoma include chemotherapy and immunological drugs which are only effective 15 % of the time. This new vaccine is not only easy to administer, but it also appears to have a much higher response rate in patients, potentially making it the best treatment option for anyone with advanced melanoma.
Just last week (April 6, 2010), scientists at the Rush University Medical Center in Chicago completed the second phase of trials for a very promising melanoma vaccine. The trial, which had stunning results, was conducted on 50 patients with metastatic melanoma, which is melanoma that had spread to multiple parts of the body. Currently treatments for advanced melanoma include chemotherapy and immunological drugs which are only effective 15 % of the time. This new vaccine is not only easy to administer, but it also appears to have a much higher response rate in patients, potentially making it the best treatment option for anyone with advanced melanoma.
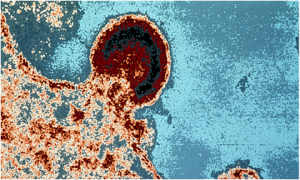
Melanoma is a rare but deadly cancer that typically begins in a mole or other pigmented tissue and can easily be removed if caught early. If it advances it is much harder to treat and without treatment the patient usually has only a few years to live.
The vaccine being tested in this study is known as OncoVEX. OncoVEX is effective because it is composed of an oncolytic virus, or a reprogrammed virus that is made to attack cancerous cells while leaving healthy cells undamaged. The vaccine is injected directly into lesions that can be felt or seen, and its ease of administration allows it to be given right in a physician’s office.
According to Dr. Howard Kaufman, the director of the Rush Cancer Program, “The vaccine worked not just on the cells we injected, but on lesions in other parts of the body that we couldn’t reach.” He explains how these injections prompt an immune response that circulates through the bloodstream to other affected parts of the body.
In the second phase of trials for OncoVEX, 50 patients were given up to 24 injections of the vaccine over the course of several months, leading to 4 partial and 8 full recoveries. The scientists found these results very promising and Kaufman stated that, “These are the best results to date for any vaccine developed for melanoma, but they need to be confirmed in a larger population.”
To confirm these results, Kaufman is set to lead a third phase of trials which will enroll approximately 430 patients from cancer centers across the U.S. These patients will be tracked for two years after their first dose and if the results are anything like the previous trial, this vaccine could turn an advanced melanoma diagnosis from a death notice into a treatable disease.
Click here for source