Obsessive-compulsive disorder, or OCD, is characterized by unwanted, repetitive thoughts and impulsive, ritualistic actions. For example, a common fear among those with OCD is a fear of germs, which results in repetitive hand-washing. While historically OCD has been difficult to treat effectively, in recent years, modifications to cognitive-behavioral therapy have had more success. Cognitive-behavioral therapy is comprised of a series of sessions between a therapist and patient to identify negative thought patterns and symptoms, and address them through discussion, exposure to stress-inducing stimuli, and practice utilizing alternative coping mechanisms to ameliorate anxiety.
While cognitive-behavioral therapy can be effective, it is time-consuming and does not work for everyone. Using functional magnetic resonance imaging (fMRIs), scientists at UCLA trained a computer analysis system to study the brains of individuals with OCD, and determine which individuals were most likely to benefit from cognitive-behavioral therapy. Their study demonstrated that if an OCD patient were to receive a seven-minute fMRI scan, the computer program could predict the success of cognitive-behavioral therapy for that particular patient, at 67-70% accuracy.
For their study, researchers recruited 42 adults with OCD. All of the participants underwent fMRIs at the beginning of the study. Then, half of the participants attended cognitive-behavioral therapy sessions lasting about 90 minutes per session, five days a week for four weeks. At the end, their brains were analyzed with an fMRI again to detect any differences in structure or brain function. The other half of the participants were put on a four-week waitlist. At the end of four weeks, having received no therapy, their brains were scanned to see if there were any differences simply due to time. These participants received cognitive-behavioral therapy treatment after the four-week waiting period.
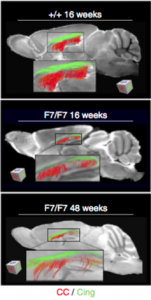
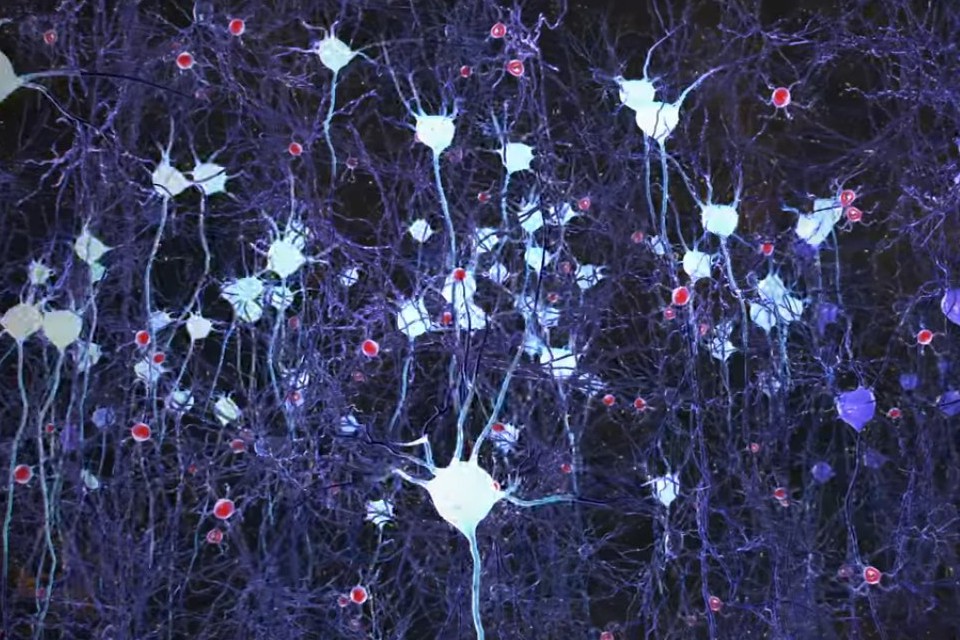
On the fMRI scans, the researchers were especially interested in studying the regions of the brain and their cellular networks that regulate attention, vision, motor skills, memory, self-evaluation, and the abstract sense of “mind-wandering,” or daydreaming, each of which play a role in development of OCD. They utilized mathematical models and computer learning to map differences between the participant’s brains, and match those results with behavior results of cognitive-behavioral therapy. They found that the computer could suggest which patients would benefit from therapy, regardless of individual symptoms or severity of symptoms.
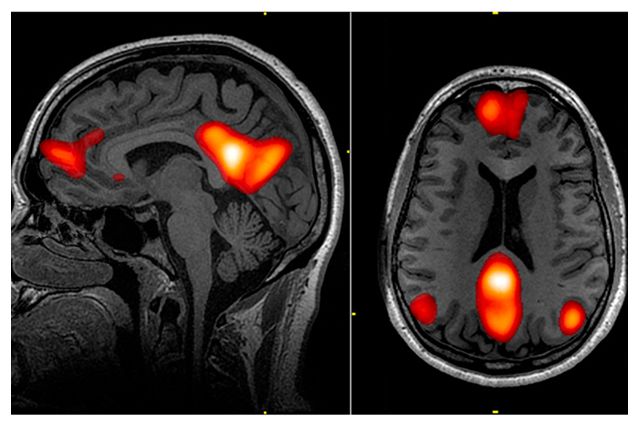
Widespread use of this predictive method would give therapists more information when deciding the best route of treatment for their patients. In the study, the researchers advocate for this fMRI computer model as a way to allocate time and resources, and direct cognitive-behavior therapy towards patients who are most likely to have success, versus other types of treatment such as medications, inpatient programs, intensive day programs, or group therapy. It is a move towards personalized medicine.
However, more research needs to be done to further advance this technique. Computers alone are not yet adequate to diagnose psychological disorders or comprehend subjective human experience. Furthermore, fMRIs are extremely expensive, and the money going towards fMRI scans could instead be put towards treatment. There is also a risk that those who the computer does not deem fit for cognitive-behavioral therapy miss out on a treatment opportunity that could actually help. While studies like this one advance scientific understanding of disorders like OCD, clinicians should proceed with caution when incorporating new computer-based evaluations that could be wrong and depersonalize the treatment experience.
Sources:
Reggente, N., Moody, T.D., Morfini, F., Sheen, C., Rissman, J., O’Neill, J., & Feusner, J.D. (2018) Multivariate resting-state functional connectivity predicts response to cognitive behavioral therapy in obsessive-compulsive disorder. PNAS [published online ahead of print]. https://doi.org/10.1073/pnas.1716686115.
Hopper, Leigh. 2018. Brain scan and artificial intelligence could help predict whether OCD will improve with treatment. UCLA Newsroom. Retrieved Feb. 5 from http://newsroom.ucla.edu/releases/brain-scan-AI-help-predict-ocd-improve-treatment.