During pregnancy, you are the reason your baby lives and it’s your job to protect your child to allow it to mature, however in the case of this patient that became near impossible. Mesenchymal hamartoma (MHCW) is a type of tumour in infants that starts at the ribs and on progresses to the chest wall.
It is very rare, only reported in just over 100 cases. Unfortunately, since the tumour is so rare, there are no published guidelines for directing doctors in treatment, and the course of treatment is highly dependent on the symptoms the patient exhibits.
For this mother and her child, it was an extreme case and doctors treated it with a very unusual course of events. However, it worked! This case had a lot of noteworthy symptoms that caused massive distress and harm to the child, as well as her mother but their approach can be very useful for future cases of MHCW. Here’s what they did.
The child was diagnosed with MHCW prenatally and began growing masses on her chest wall. The way they diagnosed the cancer was by doing an ultrasound at 33 weeks, where they noted the mass and after an MRI they found a small lesion on the right and a large lesion on the left. The left lesion was causing significant deformity in the child’s chest, with multiple ribs effected and bulging of the wall as a result. The main concern with the left lesion though was that it initiated a lot of fluid buildup and created susceptibility to hemorrhage or calcification. This means that the tumour could cause major, life threatening bleeding or could harden creating massive obstruction in the chest wall.
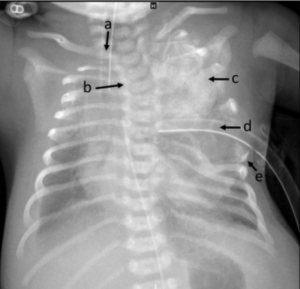
The X-ray retrieved at birth showing the affected areas. A shows the displaces trachea, B shows scoliosis, C shows the mass on the left side, D shows where the chest tube had to be placed and E slightly shows the displaced ribs. Image taken from paper cited.
Given these findings and the progression of mass growth and fetal distress, the mother had a C-section at 35 weeks. When the child was born, it was intubated for breathing support and taken to the intensive care unit immediately. Upon an x-ray that was taken, the mass on the left side showed deformity of multiple ribs, chest wall shifts and scoliosis in the upper spine. Unfortunately, after birth the mass rapidly grew and this caused issues with respiratory support for the child which majorly impacted oxygen access. Therefore, the doctors decided there was no more waiting to be done, and surgery the risk they would have to take if this child had any chance of living.

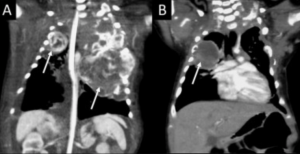
The left side (A) shows the chest wall before reconstruction, and the right (B) shows after. Image taken from paper cited.
When the infant was 15 days old, the doctors performed surgery to remove parts of the left chest wall and lung mass. After careful navigation, they successfully removed the tumour, but this showed the intense deformity of ribs 3 through 8. For the chest cavity to make room for the tumour, many heart and lung vessels were displaced, therefore the surgery took longer because of the difficult and precise guidance that needed to take place. As mentioned, the ribs were severely distorted and with the complexity of the tumour, portions of ribs 3 through 6 had to be removed and the chest wall had to be reconstructed.
After hours of surgery, the operation was successful and I can imagine how relieved the doctors and parents must have been. Given the complexity and rarity of this case, it was a massive first win.
Five days after the operation the newborn was weaned off the ventilator and began to breathe on their own. Shortly after the infant was discharged and given a protective shell that was custom made by orthotics and could be used as needed until the chest wall reconstruction became strong enough.
The first picture, A, shows the chest and left wall mass 48 hours after birth. Part B shows the successful resection of the tumour and was taken 2.5 months after surgery. Image taken from paper cited.
After 3 months, a checkup revealed that the left mass resection was a success! The right mass eventually showed significant growth and was removed once the child was a year old. Unfortunately, the mass on the left side of the chest cavity came back but was successfully removed once again.
The complications with this case and the complexity of the tumour made it very difficult for removal. MHCW is already a very rare cancer, and it did not help that the symptoms were as drastic as they were. However, the doctors that treated this patient acknowledge that their approach was risky and abnormal, but they saw it was the best chance the child had for survival and a good quality of life post-surgery.
And they were right!
This case shows how complex this cancer can be, and shows the importance of an approach that is both risky and assured. As well this case shows how important follow up appointments are considering the reoccurrence rate. An emphasis is needed on how the MHCW was removed, although it should be noted that this success does help but does not guarantee anything because of the intricacy of this type of tumour.
Source:
Groth, S., Eyerly-Webb, S., LaForest, L., Dion, E., Fisher, J., & Lillegard, J. (2020). Bilateral chest wall mesenchymal hamartoma: Prenatal diagnosis and staged surgical resection. Journal Of Pediatric Surgery Case Reports, 101474. doi: 10.1016/j.epsc.2020.101474

Alex
"This title was very eye catching! That is so interesting that such a ..."
Alex
"This is really interesting! The fact that crops and plants are damaged is ..."
Alex
"Well done, this article is great and the information is very captivating! Ethics ..."
Alex
"I was intrigued throughout the whole article! This is such an interesting topic, ..."
Alex
"This is such an interesting article, and very relevant!! Great job at explaining ..."
Grandpa
"Honey You Did a good job I will forward to my eye doctor "
murphymv
"This article is fascinating because it delves into the details of the research ..."
murphymv
"I agree, adding the photo helped solidify the main finding. "
murphymv
"This is a fascinating finding. I hope this innovative approach to improving transplants ..."
Sherzilla
"This is a great article! I would really love to hear how exactly ..."
Sherzilla
"It's disappointment that these treatments were not very effective but hopefully other researchers ..."
Sherzilla
"I agree with your idea that we need to shift our focus to ..."
Sherzilla
"It's amazing to see how such an everyday household product such as ..."
Lauren Kageler
"I will be interested to see what the data looks like from the ..."
Lauren Kageler
"A very interesting article that emphasizes one of the many benefits that the ..."
maricha
"Great post! I had known about the plight of Little Browns, but I ..."
Sherzilla
"I assumed cancer patients were more at risk to the virus but I ..."
Sherzilla
"Great article! It sheds light on a topic that everyone is curious about. ..."
maricha
"This article is full of really important and relevant information! I really liked ..."
maricha
"Definitely a very newsworthy article! Nice job explaining the structure of the virus ..."
maricha
"It's interesting to think that humans aren't only species dealing with the global ..."
murphymv
"This is very interesting and well explained. I am not too familiar with ..."
Lauren Kageler
"Great article! This post is sure to be a useful resource for any ..."
Lauren Kageler
"Definitely seems like an odd pairing at first, but any step forward in ..."
murphymv
"What an interesting article! As you say, height and dementia seem unrelated at ..."
murphymv
"Great article! I learned several new methods of wildlife tracking. This seems like ..."
murphymv
"Very interesting topic! You explained cascade testing and its importance very well. I ..."
Alex
"This article is really interesting! What got me hooked right away was the ..."
Sabrina
"I found this article super interesting! It’s crazy how everyday products can cause ..."
Erin Heeschen
"I love the layout of this article; it's very eyecatching! The advancements of prosthetics ..."
murphymv
"Awesome article! I like the personality in the writing. Flash Graphene not only ..."
murphymv
"Very interesting work! I don't know a whole lot about genetics, but this ..."
Cami Meckley
"I think the idea of using virtual reality technology to better help prepare ..."
Erin Heeschen
"I wonder if there's a connection between tourist season and wildfires in the ..."
Ralph berezan
"Not bad Good work "
Michelle
"This sounds like it would be a great tool for medical students! ..."